Sounding the alarm about obesity
By Sylvia Wrobel, Illustrations by Miguel Davilla

In 1999, in the Journal of the American Medical Association, Jeffrey Koplan and colleagues at the CDC rolled out national survey data showing an astonishingly rapid increase in obesity, male and female, across all ages, races, educational levels, and states. Whereas in 1991, 12% of adult Americans were obese, seven years later, the number had grown to 17.9%. Rarely, wrote the authors, do chronic conditions such as obesity spread with the speed and dispersion characteristics of a communicable disease epidemic.
As with most uncontained epidemics, the spread continued. By 2000, the team reported that roughly one in five adults was obese. In 1991, only four states had obesity rates of 15% or higher, but by 2000, only Colorado squeaked under the wire. From 2009 to 2010, more than a third of adult men (35.5%) and women (35.8%) were considered obese, and 56%—or "most" Americans, as Koplan put it—were overweight. His words vibrated with alarm because he knew what the numbers meant. Obesity is a major risk factor for diabetes, coronary vascular disease, high blood pressure, gallstones, osteoarthritis, breathing problems, and certain cancers, among other conditions.
|
|
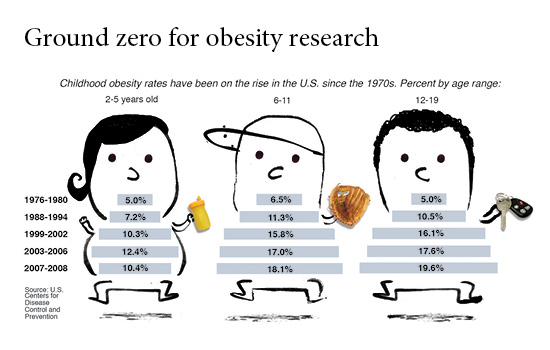
And children were not immune to the epidemic. From the 1970s to 2000, the percentage of preschool and adolescent obese youngsters doubled and that of obese 5- to 11-year olds tripled. Many already had early signs of health problems associated with obesity. Experts feared this generation might be the first to have a shorter life expectancy than their parents.
What was happening? For Koplan, the answer was and still is: We have created an environment in which the "energy in/energy expended" equation is tilting like an unbalanced seesaw. Energy in includes more high-energy foods, increased snacking, and more eating outside the home—especially in the growing fast food industry that offers increasingly bigger portions. On the other side of the seesaw, more TV time, less physical education in schools, increasingly sedentary workplaces and households, and automobiles used for all but the shortest distances are decreasing energy expended.
In 2004, the Institute of Medicine asked Koplan, by then Emory's vice president for academic health affairs, to lead a panel to develop a plan that would decrease the number of obese children and youth. Among actions the panel recommended: nutritional standards for foods and beverages sold in schools, guidelines regarding advertising and marketing to children, and expanded opportunities for healthy eating and physical activity, particularly in high-risk communities and populations. It also called for the food and beverage industry to do its part, developing healthier products and becoming more transparent about caloric and nutritional content. Two years later, a progress report, also headed by Koplan, found that government, industry, communities, schools, and families had developed many initiatives. However, most were fragmented, and few were evaluated, making it difficult to know what worked. Meanwhile, childhood obesity had increased again, from 16% to 17.1%. Fully a third of American children and youth were already obese or at risk of becoming obese.
An economic epidemic
In 2004, Emory's Kenneth Thorpe began looking at obesity's impact on health care spending and the economy. It was a job made for Thorpe, Woodruff Chair of Health Policy and Management at the Rollins School of Public Health (RSPH), who was used to startling health cost statistics. But what he found surprised him.
|
|
Using surveys of health care spending for the U.S. population and calculating the body mass index (BMI) of respondents based on self-reports of height and weight, Thorpe found that rising obesity rates and treatment intensity accounted for 27% of the growth in inflation-adjusted per capita health care spending between 1987 and 2001. The growth was attributable to the rise in both prevalence and treatment costs for obesity-related diabetes, hyperlipidemia, hypertension, and heart disease. In 1987, based on 2001 dollars, obese people spent 15.2% more per capita on health care than normal weight people. By 2001, it was 37% more.
Thorpe believed putting such numbers out there would be half the battle in persuading government, policy makers, and business leaders to take up the battle against obesity. The researchers themselves funded a follow-up study, which found that between 1987 and 2002, the cost to private health insurance of treating conditions linked to obesity had increased tenfold, from $3.6 billion to $36.5 billion, a direct reflection of the rising number of obese patients, not of rising treatment costs per patient.
Thorpe's 2007 study, a first of its kind, showed that Americans ages 50 and older were more likely than their European counterparts to be diagnosed with heart disease, high blood pressure, high cholesterol, stroke/cerebrovascular disease, diabetes, chronic lung disease, asthma, arthritis, osteoporosis, and cancer. Although the research team noted possible explanations, such as more aggressive diagnosis and treatment, they ultimately concluded that the United States was spending more because its citizens were less healthy. And they were less healthy, in large part, because they were obese at nearly twice the rate of Europeans. "If the U.S. could bring its obesity rates more in line with Europe's," wrote Thorpe, "it could save $100 to $150 billion per year, a reduction of 12.7% to 18.7% of the total budget for personal health care spending among those ages 50 and older."
New data compiled by Thorpe's team as part of the 2009 America's Health Rankings was the first to estimate obesity prevalence and costs at the state and national level for the next decade. The news was not good. If current trends continue, it said, by 2018 more than 43% of the U.S. adult population will be obese, and obesity costs will quadruple. In Georgia, direct health care costs related to obesity would rise from $2.5 billion a year in 2008 to nearly $11 billion by 2018.
"Current approaches to controlling health care costs are not working," says Thorpe, "because they ignore the true drivers of those costs. If Congress, insurers, and employers are serious about reining in health care spending, then obesity prevention needs to be at the top of their agenda."
|
Body Mass Index (BMI) is determined by weight and height and correlates, in most adults, with body fat. A BMI of 18.5 to 24.9 is considered healthy, 25 to 29.9 overweight, and 30 or higher, obese. By this calculation, a 5'9" adult is healthy at 125 to 168 pounds; overweight at 169 to 202 pounds; and obese at 203 pounds or higher. See cdc.gov/obesity/defining.html. |
Diabetes: the other epidemic
When researchers and policymakers speak of the health and economic impact of obesity, whether in Atlanta or worldwide, increasingly their focus lands on type 2 diabetes, for which obesity is a strong risk factor.
In 2011, 25.8 million Americans had diabetes. Another 79 million are considered pre-diabetic based on blood glucose levels, putting them at risk to develop diabetes within five to 10 years. That comes to roughly a third of the U.S. population. One in five health care dollars goes to treating diabetes, as does 25% of Medicare's annual budget. No longer just a rich-country disease, diabetes is on the rise in every country in the world. Of the 366 million people with diabetes worldwide, 80% live in low- and middle-income countries, with a spread across urban and rural areas.
K. M. Venkat Narayan, Ruth and O. C. Hubert Chair of Global Health and Epidemiology at the RSPH and a professor of medicine in Emory's medical school, and his colleagues are building a worldwide coalition to find a global solution to this epidemic. They are beginning with shared research and training programs between Emory and various organizations in India, where type 2 diabetes has increased 72.3% over the past 14 years in cities like Chennai.
The population and individual differences that Narayan sees have convinced him that "the causes of obesity are a lot more complex than the first law of thermodynamics, not simply a matter of energy-in and energy-out. We need more research into causation of obesity and diabetes," he says, "but we also need to work with what we already know."
His partnership does both: studies of 12,000 people in India and Pakistan investigate causes of type 2 diabetes, especially in cases that occur at lower BMI and/or at younger ages, as well as diabetes's close cousin, cardiovascular disease. More than 600 people with prediabetes are involved in a clinical trial aimed at preventing type 2 diabetes, and another 1,200 participants with diabetes are participating in a study designed to improve care and prevent complications.
Lowering statewide cancer risk
Obesity is a risk factor for some cancers, especially postmenopausal breast cancer and colon cancer. Michelle Kegler—director of the Emory Cancer Prevention Research Center, an expert in community participatory research, and a behavioral scientist at the RSPH—is working with the Cancer Coalition of South Georgia and three community health centers near Albany and Valdosta to test an intervention to prevent weight gain in women ages 35 to 65. Local residents trained as coaches meet regularly with the women over five months, helping them make their homes more supportive of healthy eating and physical activity. The 500-household study has just begun, but an earlier pilot suggested that the intervention was successful in increasing the number of fruits and vegetables in the house, lowering dietary fat, reducing hours spent eating in front of the television, increasing exercise time, and lowering weight. If the randomized control trial works as well, the team plans to expand it widely.
Reducing pediatric liver disease
Seventeen percent of all U.S. children and one in three of overweight children have nonalcoholic fatty liver disease (NAFLD), a rise in prevalence that mirrors the rise in childhood obesity. Most are 12 years or older, but in the liver disease clinic at Emory-Children's Center, pediatrician Miriam Vos sees patients as young as seven. Based on longer-term studies in adults, she worries that these youngsters' conditions will progress to cirrhosis, liver cancer, liver failure, or 20 years from now early strokes or heart attacks. Vos suspects childhood NAFLD is tied to a diet high in sugar or fructose, such as that in sweetened beverages and processed grains. In 2008, using data from a national nutrition study, Vos found that sugar and/or fructose accounted for 12% of calories consumed by children. Subsequent research shows glimmers of hope: sugar consumption has declined somewhat, perhaps because of increased public awareness and more nutritional labeling. This matters. Children's liver enzymes improve when sugar consumption goes down and physical exercise goes up. While continuing behavioral research, Vos and her colleagues also are enrolling obese children with severe NAFLD in an NIH clinical trial that tests a new medication.
|
|
Changing outlooks
Realizing the true scope of the obesity epidemic and its impact on population health and the economy seems to ignite a crusading instinct. Koplan has continued to lobby the government to ensure public access to nutritional information and the food and beverage industry to market healthier products, at home and globally. He has joined the board of the Robert Wood Johnson Foundation, which has invested $500 million to fund literally hundreds of childhood obesity intervention projects and studies on providing access to affordable healthy foods and increasing opportunities for physical activity in schools and communities.
In 2007, Thorpe helped form the Partnership to Fight Chronic Disease to position obesity and related chronic illnesses as a top health care priority in the upcoming presidential election. He serves as executive director of the partnership, a coalition of patient, provider, business, labor, and other groups.
Evaluate first, says Thorpe. Then fund programs that work. That makes common economic sense. For example, he calculates that it would take $80 million to put a proven 16-week lifestyle intervention program in every YMCA in the country, enrolling every overweight and prediabetic person between 60 and 69. Program funding would come from existing federal dollars in the Prevention and Public Health Fund, with Medicare saving between $20 and $30 billion over the lifetime of those individuals.
In a perspective article in the New England Journal of Medicine last fall, several Emory public health experts, including Narayan and Koplan, again cited the need for a collective global effort to tackle noncommunicable diseases such as those caused by obesity. They drew parallels to lessons learned in the HIV/AIDS epidemic. One, that research, prevention, and treatment efforts must be global rather than national. Two, that prevention must be linked to early diagnosis and treatment, connecting community resources with organized health care systems. And three, prevention efforts must integrate both behavioral and biomedical approaches.
|
|
Cardiometabolic disease—Clinicians also have taken up the fight. Over 30 years, Emory heart surgery professor Omar Lattouf has operated on more than 10,000 patients. Three years ago, reviewing data on these patients, he could clearly see a constellation of problems that make up cardiometabolic syndrome: obesity, especially abdominal obesity; elevated blood pressure, triglycerides, cholesterol, blood glucose, and inflammation; and insulin resistance. Each factor aggravates the other. Having several risk factors markedly raises a person's risk for heart disease and diabetes. Lattouf's study went further. He found that the syndrome played "real havoc" with his surgical patients, making those with more factors more likely to require longer postsurgical hospital stays, spend more time on a ventilator, need blood transfusions, and experience more postsurgical complications. At an eight-year follow-up, there was an 11% negative difference in survival in patients meeting the World Health Organization criteria for metabolic syndrome, which include diabetes plus any two of the following risk factors: high blood pressure, obesity, or abnormal blood lipids.
Lattouf continues to investigate (he is now looking at all heart patients at Emory, not just surgical patients). But like Koplan, Thorpe, and frequent co-investigator Narayan, Lattouf also wants to bring more attention to this condition that now affects more than 300 million people worldwide, including 25% of Americans—numbers likely to rise as the population ages. His reach is wide. He heads the Global Coalition to Combat Cardiometabolic Syndrome, which holds scientific meetings and designs curricula to prevent obesity in schoolchildren. This year the American College of Cardiology selected Lattouf's proposal for a multinational collaboration to study the impact of cardiometabolic syndrome on health care and economics, announcing the launch of the "Save a Million Hearts Campaign"
in March.
Childhood obesity—Children's Healthcare of Atlanta's investment in reducing and preventing childhood obesity in Georgia has been nothing short of amazing, says Stephanie Walsh, the Emory pediatrician who serves as medical director of Child Wellness at Children's. She believes that Children's new Strong4Life movement is powerful on multiple levels, from specialized treatment programs to year-long programs for families struggling with weight issues, from summer camps and training programs to materials to help Georgia clinicians who perform well-child exams talk more easily about weight, nutrition, and exercise. The campaign also is building a continually growing number of partnerships with schools, day care centers, and community organizations like the YMCA, Boys & Girls clubs, Head Start, and the federal WIC grant to states for supplemental food program. Strong4Life's mantra is: It took 30 years to get us all talking about childhood obesity. Now let's work together to solve the crisis.
Another strength, adds Emory pediatrician Vos, director of research for child wellness, is Strong4Life's research-based programs. Forty percent of Georgia's children may be overweight, more than in any state except Mississippi, but Children's research found that some Georgia parents did not see their child's obesity as a problem. That's why Strong4Life began with a controversial wake-up call: hard-hitting TV spots and billboards that feature overweight children with taglines such as "Chubby isn't cute if it leads to type 2 diabetes." Ongoing programs respond to research showing parents need more information on prioritizing efforts to help their overweight children. Its programs offer clear "baby steps" such as decreasing sugar drinks and increasing consumption of water, vegetables, and fruits, along with less TV and more physical activity.
Next steps
|
|
According to National Health and Nutrition Examination Surveys, the rate of increase in obesity appears to have slowed during the past decade and may be reaching a plateau. However, with a prevalence of 35.5% among adult men, 35.8% among women, 18.6 % among boys, and 15% among girls, these numbers are still a long, long way from the Healthy People 2010 goals of 15% adult obesity and 5% child obesity in the population.
So where does that leave us? In Georgia, the Department of Public Health has made tackling the state's high obesity rate a top priority. It is working to implement the Georgia SHAPE (Student Health and Physical Education) Act, a public-private partnership to promote childhood fitness and build a culture of wellness. And each year, with funding from the CDC, it collects health information, including height and weight, in a state-based phone survey of more than 400,000 adults to identify obesity prevalence.
At Emory, faculty are continuing their efforts to confront the challenge head-on. Researchers are trying to identify contributing factors, such as intestinal bacteria, hormones, genes, cellular changes, specific diets, and psychosocial factors. Clinicians, economists, and public health researchers are searching for key findings to identify which interventions work. Together they are looking to turn around a costly obesity epidemic that spans genders, ages, races, educational levels, and countries.
Related Links:












