In Tune to a Different Rhythm
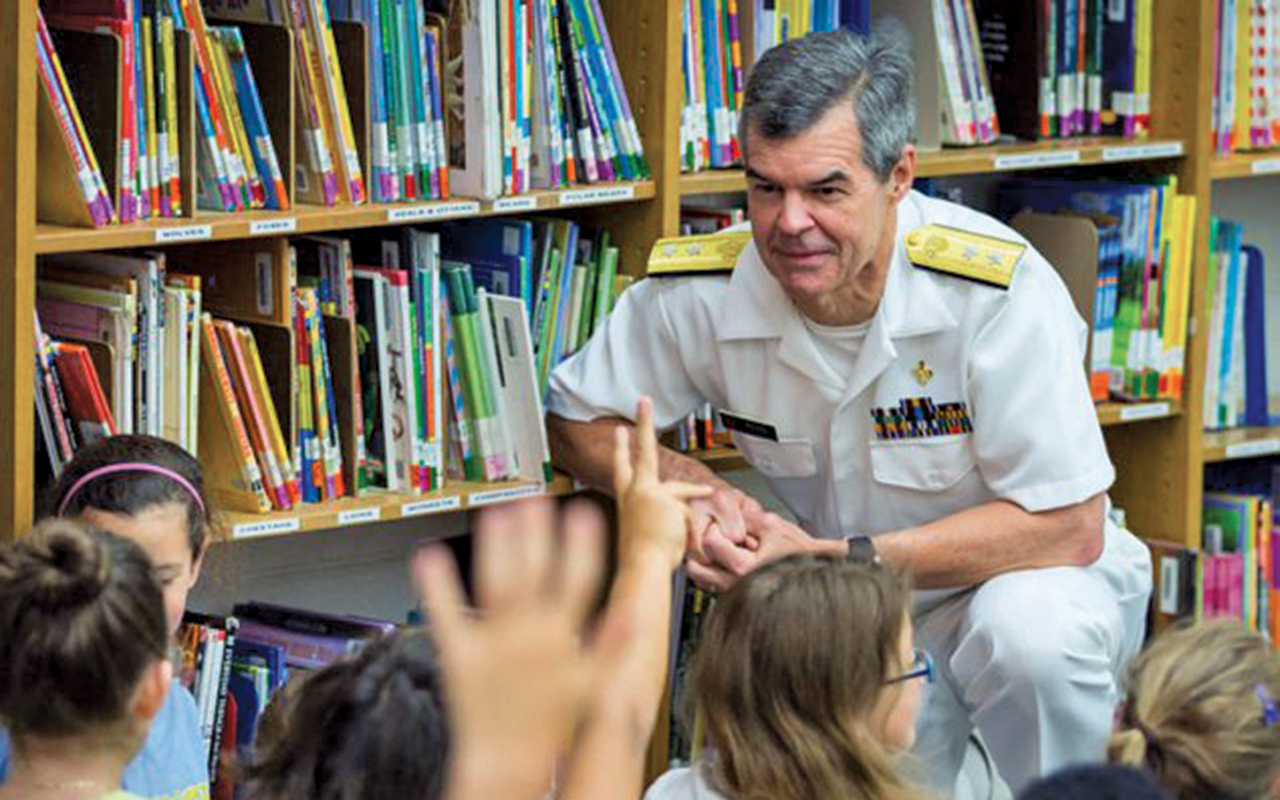
As Deputy Director for Public Health Service and Implementation Science at the Centers for Disease Control and Prevention (CDC), Rear Admiral Stephen C. Redd 83M spent March 11 testifying during a House Homeland Security Committee hearing on “Confronting the Coronavirus: The Federal Response.”
“As we begin to see community spread of this virus, it will be important for all of us to take action in preventing its spread through common sense public health precautions,” Redd told the committee on the day the virus’s spread was declared a pandemic, in the hearing covered by C-SPAN.
Redd had been thinking about such a threat for a while. In a podcast for the National Association of County and City Health Officials that aired in August 2019, Redd talked about the health threats that keep him awake at night: an influenza pandemic, other contagious respiratory disease outbreaks, and weather disasters related to climate change.
Redd’s words were prophetic given the events of 2020: the coronavirus pandemic, wildfires in California, and powerful hurricanes. “The nature of our work is to be ready for the threats we can identify and be able to pivot to respond to events that are of even greater consequence,” said Redd in the podcast. “When we’re in an emergency response, we can fail to accept or appreciate the uncertainties,and we think we know more than we do. Maintaining a sense of humility and contingency is really important.”
Redd is poised to retire from CDC this year. One lesson he has carried with him throughout his 35-year career is that medicine and public health have distinct tempos.
He became aware of the difference following his second year of study at Emory School of Medicine, when he held a summer job in CDC’s reproductive health division. He happened to work there in 1981, when the first cases of AIDS were diagnosed. “CDC was a much smaller place then,” says Redd. “Even though I didn’t work on HIV, I was able to attend lectures on pneumocystis and Kaposi’s sarcoma. Everyone at CDC was trying to figure out how to deal with the growing AIDS epidemic. It gave me a taste of something different that I could do with my medical degree.”
Redd went on to graduate from Emory and complete a medicine residency at Johns Hopkins University School of Medicine. In 1985, he returned to Atlanta, his hometown, and CDC to serve as an officer with the Epidemic Intelligence Service (EIS). For some time, he also volunteered as an attending on the medicine service at Grady Memorial Hospital.
“There was a different rhythm at CDC,” Redd says. “During my residency and at Grady, I stayed up nights taking care of patients The hours were long and the feedback from patients was immediate. As an EIS officer, I investigated disease outbreaks, which was totally different.”
Shortly after completing EIS training, Redd traveled to West Africa to assess the feasibility of conducting a pneumococcal vaccine trial in Senegal. Following EIS, Redd remained at CDC, leading childhood survival projects (acute respiratory infections and malaria) in Africa and efforts to eliminate measles in the United States (achieved in 2000). When terrorists attacked the US in
2001, Redd was working in CDC’s National Center for Environmental Health to reduce the burden of asthma. A few weeks later, he was on a charter plane to Trenton, New Jersey, to assist with the emergency response to the anthrax attacks following 9/11. Letters containing anthrax had been sent from a Trenton post office and thus put its workers at risk. The response brought home another important lesson for Redd: knowing when to pivot.
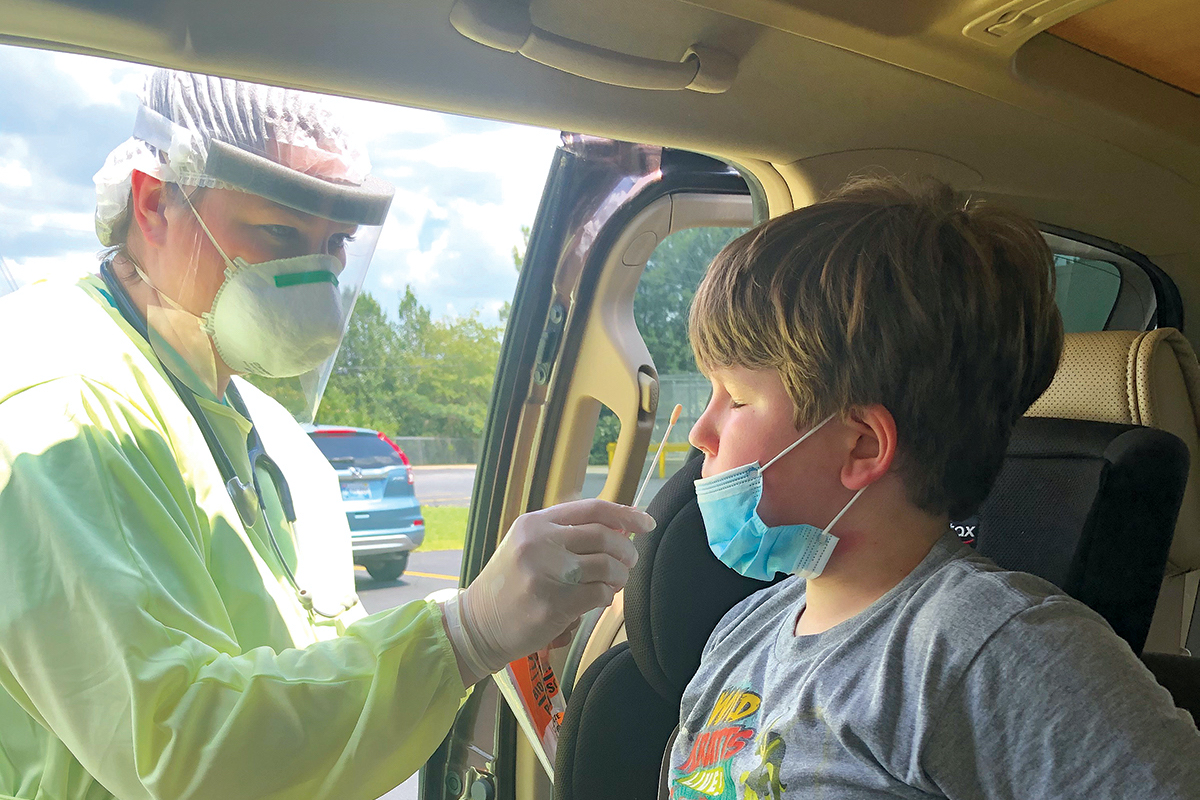
“On our first day in New Jersey, a Sunday, we went to the post office and swabbed the noses of employees who had worked there,” he says. “The next day, we learned that all the tests were negative and that our method for determining exposure was inadequate. We then contacted hospitals in New Jersey and asked them to send a daily report of suspected cases of anthrax, either from the emergency room, the intensive care unit, or the laboratory. We developed questionnaires that the hospitals completed and faxed to us every day. That made it easier to determine if anyone had been exposed and get them on treatment as quickly as possible.”
Redd’s response skills would be further tested as director of the Influenza Coordination Unit. CDC formed the unit in 2006 based on national and global concerns that the H5N1 avian influenza virus could become a human pandemic. At the time, the virus had spread in birds from Asia to Africa and occasionally in people. The human mortality rate was 60%.
“The spread of the H5N1 virus in humans was unprecedented and led to a global effort to prepare for a possible pandemic,” says Redd. “CDC was on the leading edge of that effort. That’s when the Influenza Coordination Unit was formed.”
Its first rule of operation: practice, practice, practice. Working with ex-military experts, CDC staff wrote a response plan grounded in different exercise theories. In 2007 and 2008, the unit conducted five real-life exercises in the agency’s Emergency Operations Center.
During each exercise, a group of experts worked “behind the curtain,” injecting information to which staff had to respond. “We set up our daily rhythm,” says Redd. “We held mock press conferences and daily briefings, knowing that the scenario could change at any moment. Through those exercises, we learned a lot about what we would have to do during a real pandemic.”
In 2009, when the first cases of H1N1 influenza were reported, CDC went into action. “We activated the Emergency Operations Center but still weren’t sure how severe the disease would be,” says Redd. “The first two patients in the US had already recovered by the time they were identified. We suspected there was widespread transmission but didn’t know the severity.”
The seminal moment occurred late on a Thursday afternoon when CDC received a report from Canada where specimens from people hospitalized in Mexico had been tested and confirmed as H1N1 cases. “Some of the people who subsequently died were among the cases,” says Redd. “There was more severe disease in Mexico than we had seen in the US. From that moment on, everything changed.”
Emergency responses, drill sessions and real ones, highlight perhaps the biggest challenge of all—making a decisive call to protect individuals and populations.
“The reality is you have to make decisions without having all of the information that you would like to have,” Redd explains. “If you delay, that’s a decision in itself—it’s deciding not to do something. There’s a timeframe for every decision, from martialing the best evidence you have to making a decision when it has to be made.”
Two decades have passed since measles was eliminated in the US. Yet measles cases have resurged in recent years. In 2019, more than 1,000 cases were confirmed in 31 states—the highest number since 1992.
Key factors are driving the increase. Although global measles control has improved immeasurably, the disease is still common in many countries. Unvaccinated travelers to those countries bring the disease back to the US, where it spreads easily among unvaccinated people. Many have avoided immunization, believing it is unsafe.
To combat the resurgence, CDC has taken steps to remove financial barriers to vaccination and provide constant assurance that the MMR (measles, mumps, rubella) vaccine is safe and effective. “The vaccination coverage for measles has been over 90% in the past 15 years or so,” says Redd. “Ultimately, the global elimination of measles is the answer to ending the outbreaks we are having here. It’s hard to say how soon that day will come. As long as measles can be imported, we’ll be at risk in the US.”