Aging with HIV
By Marlene Goldman
Marianne Swanson: Nurse, patient advocate, grandmother
Marianne Swanson remembers well when the diagnosis of HIV was a death sentence. The virus killed most of her young family.
It was 1987, and the wife and mother of two sons was beside herself as her youngest, two-year-old Joshua Paul, grew sicker and sicker. He developed a host of scary and confusing symptoms, including swollen lymph nodes that turned out to be cancerous. Two weeks before he died, he was tested for HIV.
|
|
"No kids were being tested for HIV then, but because of my husband’s past and his risk factors, we asked for the test," says Swanson, a nurse, who was pregnant with her third child at the time. (Her husband had told her that he had struggled with his sexuality in the past and had had an affair with a man.)
"Joshua Paul died in July, and in August I got a call from the doctor that he had tested HIV positive and that the whole family needed to be checked," she says.
Those tests brought more devastating news: Swanson and her husband both had HIV. Only three-year-old Jonathan was spared.
Their third child, a girl they named Annalisa, was born with full-blown AIDS, a medically fragile child who spent half of her short life in the hospital. She was 17 months old when she died.
"We tried everything to save her, even enrolled her in a National Institutes of Health study, but she lost her battle with HIV in May 1989, when there was really no therapy for anyone, let alone children," Swanson says.
HIV combination antiretroviral therapy was introduced in the summer of 1996—too late for Swanson’s husband, who died two days before the Olympics opening ceremony in Atlanta.
"I never blamed him, to be honest, because I saw the way he suffered. He saw the two kids die. He did not need the burden of a wife blaming him. He didn’t need me to say it," she told CNN, in a previous article about her experiences.
Swanson, whose life was saved due to the new therapeutic drugs and who now works with HIV patients at Atlanta’s Ponce de Leon Center, decided to speak publicly about her experiences to battle the stigma that can still accompany the disease.
"It’s quite sad but a miraculous kind of story because I survived through all that and I’m living a totally different life now," she says. "I have suffered my losses, but I not only survived, I thrived in the setting of HIV."
It is strange and wondrous to her, even now, to be thinking about aging. "A lot of people who have survived as long as I have remember the time when we were literally dying or waiting to die, and we are now living and aging just like everyone else. Getting older is a good problem to have—I’m overjoyed to be aging," she says.
When her surviving son graduated from high school and enrolled in Georgia Tech, Swanson took a job with the Grady Hospital Infectious Disease Program, at the women’s clinic, then transfered to the main clinic. She first visited Grady Health System’s Ponce Center as a patient. Now a senior staff nurse, Swanson has spent more than a decade talking to HIV-positive men and women about how to live with the disease.
Sometimes she bridges the gap between herself, a 58-year-old Italian woman, and her younger patients, many of them African American men, by sharing her own experience.
"HIV is the great equalizer, no matter your age or background," says Swanson.
"I don’t think my older patients struggle as much with HIV as my young men do. HIV is too big for them. They don’t have the skill set to navigate the public health system. I have patients who weren’t even born when I contracted HIV."
When a patient’s HIV status is compounded by homelessness, substance abuse, or other difficulties, Swanson is called upon to be their champion and cheerleader, lobbying for them, encouraging them, and cajoling them to return for check-ups and stay on their meds.
Some need to be reminded that it can be a fatal illness.
"They were born in a day and age of HIV treatment; they don’t know the death stories," she says.
Swanson has remarried and between her and her husband, Darrell, they have six children and seven grandchildren. Surviving long enough to be a grandmother was an unexpected joy.
Sometimes, she feels that she is aging better than many of her HIV-negative counterparts because of the diligence required.
"I have a life-threatening illness so I have to pay attention to my health," she says. "I see my doctor three or four times a year, I get my blood pressure and mammogram done. I get my blood work, I know what my cholesterol is."
She takes four pills a day for her HIV (fewer than in the past, with fewer side effects), a drug to control her cholesterol, a baby aspirin, multivitamins, calcium, and vitamin D for her bones.
"A lot of us who have survived for 25 or more years, we don’t take this for granted," she says. "We understand the gift we have been given, because a lot of our loved ones, partners, and friends did not survive to see it."
The Ponce Center: HIV and diseases of aging
Until about five years ago, much of HIV/AIDS research focused on treatment.Now, patients have access to a combination of easily tolerated, convenient medications that promise to keep viral loads suppressed for decades.
|
|
So the research focus has radically shifted to looking at chronic conditions or diseases that often accompany long-term HIV.
Grady Health System’s Ponce de Leon Center, one of the largest and busiest HIV centers in the country, provides care and support services to 5,000 men, women, and children living with HIV/AIDS. These patients are living well beyond what was once only dreamed of, but that has presented its own complications, including early onset of illnesses associated with aging.
"We see patients with heart disease, strokes, thinning of bones, hip fractures, and cancers at a younger age than they would otherwise expect," says HIV researcher Jeff Lennox, professor of medicine at Emory, and associate chair for Grady affairs.
This might be due to inflammation, antiretroviral therapy itself, or classic behavioral risk factors like smoking, he says. One study showed that HIV patients on antiretroviral therapy who smoked lived an average of 12 years less than those who didn’t smoke. "In the past, there really wasn’t a strong motivator for patients with HIV to quit," he says. "But now that people are living longer with HIV they are suddenly having to come to grips with stopping smoking."
HIV-positive populations also tend to have higher rates of heart disease, which is probably due to a combination of smoking, the virus itself, and HIV medications that can elevate lipid levels.
Certain types of cancers—rectal, lymphoma, and liver cancer in patients infected with hepatitis B and C—also occur at a higher rate in HIV patients.
Researchers have also noted an increasing prevalence of cognitive impairment in HIV-positive adults. Some evidence indicates that virus replication in the brain is not as easily controlled as in the rest of the body, perhaps because medications cannot easily penetrate the brain.
For patients with long-term HIV, doctors must tease out these multiple variables. "It’s a very complex area, when a patient starts to notice problems," Lennox says. "Are these problems due to aging, HIV, medications, or something else?"
Richard Rhodes: AIDS Activist, Navy veteran, AARP member
Richard Rhodes’s birthday present to himself the year he turned 65 was an HIV test at AID Atlanta.
He’d been getting the test every year on his birthday since the organization was founded some 15 years earlier. This time, he was HIV positive.
|
|
At first he shared the news with just a few friends and those who needed to know, but in recent years, the 77-year-old Atlantan has been publicly sharing his experiences with HIV and promoting the need for everyone to be tested.
"It doesn’t make any difference how old you are," he says. "All people should practice safe sex and everybody should have an HIV test at least once a year, whether they are at risk or not, because you never know. You can’t judge a person by how they look."
Educating others about HIV is consistent with Rhodes’s long history of championing social and political causes.
After moving to Atlanta in 1972, he became the first openly gay candidate to run for the Georgia House in 1988, the first openly gay delegate to the Democratic National Convention from Georgia the same year, and the first to serve as chair of the DeKalb Democratic Party.
A founding member of SAGE (Services and Advocacy for GLBT Elders) in Atlanta and the Atlanta Prime Timers, a social group for age 40 and older gay and bisexual men, he received a Lifetime Achievement Award from the Atlanta Gay and Lesbian Chamber of Commerce.
Today, as an AARP (American Association of Retired Persons) volunteer, Rhodes also frequently speaks to groups about the advantages of membership in that organization, such as political leverage.
Rhodes feels fortunate to have been diagnosed with HIV later in life when medications were better, unlike many people he knew who were hit by the first wave of HIV/AIDS.
"Sometimes they died within a week of being diagnosed," he says. "There was only one drug, AZT, and it was pretty toxic. There were times when I was going to at least two funerals a week."
In the beginning of the epidemic, he kept a list of people he knew personally who had died of HIV. "But when it reached 100," he says, "I just shredded the list and said I’m not going to worry about this anymore."
Now, he says, HIV is "pretty much like any other disease—if you take good care of yourself and take your medications, it’s controllable."
In recent years, though, Rhodes has dealt with other serious health issues: stage 3 kidney disease, diabetes, and a triple bypass. "So I don’t even worry about AIDS," he says.
The veteran, who served in the U.S. Navy in the late 1950s aboard the USS Lexington stationed out of San Diego, makes regular visits to the Atlanta VA Medical Center for treatment.
He’s one of a growing number of older veterans who receive treatment for HIV there.
"I see a kidney specialist, someone for diabetes, a heart specialist, an infectious disease specialist, and a dermatologist—they keep me running well," he says. "I spend a third of my income on medications and doctors, but that’s the life I live and I’m very happy to be alive. "
Rhodes’s parents lived into their 90s and his infectious disease physician tells him he has a good chance of reaching that milestone as well. Good genes and treatment aside, Rhodes attributes his longevity to attitude.
"HIV hasn’t limited me in any way," he says. "I wake up every day and take my diabetes medication and other meds, but I don’t even think about having HIV, maybe because I don’t have any bad symptoms. In spite of all the things that are wrong with me, I live life to its fullest."
The Atlanta VA Medical Center: HIV and Aging Veterans
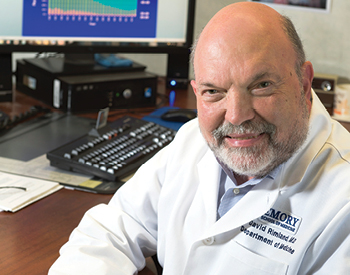
The Atlanta Veterans Affairs Medical Center (VAMC), which serves 1,600 HIV-positive patients, has the largest HIV patient population of any VAMC in the country, and the median age of these patients is 52.
|
|
Guidelines in place since 2009 require testing everyone serving in the military for HIV. Also, the military has not accepted HIV-positive recruits since 1985, when testing became available. "So between these two things, we have this older age group who is being found positive," says David Rimland, chief of infectious diseases at the Atlanta VAMC and Emory professor of medicine. "We’re also diagnosing more people in their 60s and 70s. Older people are having sex but may not know that they are HIV-infected or that their partner is infected."
The VA has been proactive about getting HIV-positive patients into care and on medication, following up to make sure they have no detectable virus, and providing counseling. In turn, mortality rates decreased from 25.9 per 100 veterans in 1994 to 1.2 per 100 veterans in 2012. "We’ve done a great job of keeping people alive," Rimland says. "This older population is doing very well from an HIV standpoint."
But now, they are dealing with other diseases as well as the challenges of retirement and old age. "Can you imagine if you were diagnosed 20 years ago when you were 40? We didn’t have much to offer back then, in terms of treatment, so you thought you would be dead in five years," he says. "Then suddenly you're doing great, you're getting older, and you hadn't planned on that at all."