Learning to Love Our Bugs
By Jerry Grillo, Illustrations by Giulia Ghigini

Each of us is a mobile ecosystem teeming with trillions of living organisms.
They live on us and inside us, surround us like an invisible cloud, maintain and sustain us, ignore us, occasionally attack and kill us, and, ultimately, define us.
The human microbiome is made up of bacteria, fungi, viruses, and the like, and they cover every surface of our bodies.
"These microbiota are mostly in your gut, but also in your mouth, on your skin, in your lungs," says Emory biologist Nicole Gerardo. "They're playing critical roles in how you interact with the environment, how you process food, how you fight off pathogens, how you interact with drugs."
Some of our remarkably fertile microbes are identical to those that live in other humans. But many are a distinct reflection of our individual experiences, shaped by who or what we've touched, where we've been, what we've breathed, and what we've consumed.
 |
"Research interest in the human microbiome is exploding now," says Gerardo, who gave the introductory presentation at Emory's first microbiome symposium in November.
Spurred on by ambitious efforts like the National Institutes of Health's Human Microbiome Project, such research is demystifying the role of our myriad microbial passengers.
"It's like we're entering a new frontier of science, something that was basically ignored by medicine for a long time," says infectious disease researcher David Weiss, director of Emory's Antibiotic Resistance Center. "We're really at the beginning of studying all this, but I do think that in our lifetime, we'll be able to monitor each person's microbiome and intervene to improve their health. Looking at what type of bacteria we have and how resistant or sensitive they are to drugs will be an important part of health care. Most of the bugs we tote around are helpful, but they can also be ticking time bombs."
In this case, we may be able to someday diffuse the situation, replacing pathogenic microbes with a friendlier variety.
"There's great promise in manipulating the microbiome, in actually changing it," says geneticist Michael Zwick. "Actually, it's already happening."
|
"Your gut gets disrupted and barren from antibiotic use," says Colleen Kraft, the granddaughter of two farm families. "I think of a garden analogy, or a pasture that gets decimated in winter. When our gut is decimated, using more antibiotics to treat the bad bacteria doesn't work." |
You do what?
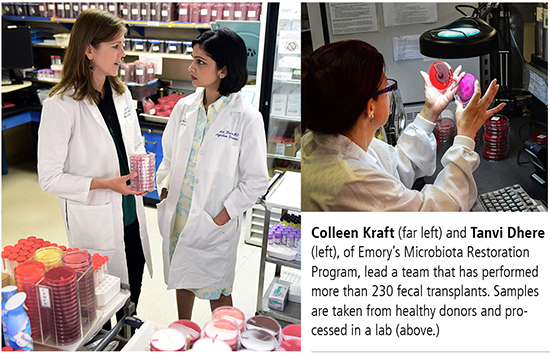
Pathologist Colleen Kraft has grown used to the responses she gets in social gatherings when she brings up her work with fecal transplantation, in which gut microbes are transferred from one person to another.
"It's been a great conversation starter at parties when people ask me what I do or what my research interests are," says Kraft, an infectious disease physician who launched Emory's fecal transplant program in 2012. "But I don't get as much laughter or as many funny looks now as I did back then."
A growing awareness of the microbiome's influence is reflected in record sales for probiotics—friendly bacteria used as a form of preventive medicine that now show up in everything from yogurt to over-the-counter supplements.
While probiotics can be used by healthy folks to restore good bacteria after a bout of antibiotics, patients who develop the potentially fatal bowel infection Clostridium difficile (C. diff) may require a fecal microbiota transplant.
Kraft and gastroenterologist Tanvi Dhere are co-directors of Emory's Microbiota Restoration Program. They lead a team that has performed more than 230 fecal transplants with an overall success rate of 98 percent.
Kraft recruits donors and maintains a stool bank, while Dhere performs and manages fecal transplant procedures.
A small fecal sample is taken from a healthy donor, processed in a lab, and transplanted into the patient's colon, where the new, healthy bacteria can restore microbiotic balance to a compromised digestive system.
"Your gut gets disrupted and barren from antibiotic use," says Kraft, the granddaughter of two farm families. "So I think of a garden analogy, or a pasture that gets decimated in winter. When our gut is decimated, using more antibiotics to treat the bad bacteria doesn't work."
 |
A fecal transplant remains the gold standard when it comes to treating C. diff, which affects more than 450,000 people every year, killing about 29,000.
"A lot of my friends take probiotics, but that's not as efficacious as poop, which is hundreds of thousands of times more effective than typical probiotics," Kraft says. "Poop is the ultimate probiotic."
Microbes run amok
About 1,000 species of microorganisms jockey for position in our gut at any one time. Mostly, they're cooperative and helpful bugs, protecting us from pathogens with their sheer mass—there's hardly room for anything else in such a crowded community.
They boost our immune system, help keep us fit and slim, and typically exert their microbial beneficence throughout the body.
Sometimes, however, a normally harmless microbe can run amok if your system gets thrown out of whack by, say, an antibiotic or steroid. That's what happened to Gail Swanson.
About a week after returning home to Atlanta following a mission trip to Peru in June 2014, and following two trips to the emergency room with what initially was diagnosed as renal failure, Swanson was told she had C. diff. She was prescribed antibiotics and the infection subsided for a while and then returned—the beginning of a wretched cycle in Swanson's life.
"I was as sick as could be and thought, 'What hope do I have?' It felt like I was going to be like this for the rest of my life, weak and tired," says Swanson.
Her gastroenterologist told her the infection would probably go away on its own. And it seemed to, after four months of struggle.
But last summer, following a course of antibiotics to treat a sinus infection, C. diff returned. Her physician, as many do, prescribed more antibiotics, "and I wound up in the ER with C. diff yet again," she says. "That's when I decided that I had to find another option."
A Google search led her to information about fecal transplants. "I thought, 'Yuck,' but I was desperate," Swanson says.
She was enrolled in a clinical trial at Emory testing an alternative to traditional fecal transplants—a "poop pill" designed to tease out the specific bacterial spores involved in treating C. diff. Initially, she was placed in the control group, which received the standard treatment, a powerful and expensive antibiotic called vancomycin.
"It did make me feel almost human again," says Swanson, who has four daughters and four grandchildren.
But the C. diff came back, which was expected. Finally, Swanson was given the real stuff. She calls it, "a miracle. Within two days, the C. diff was gone, and I was dancing in the streets."
"The thing of it is," she says, "I've always suffered a little bit from depression, but I must have gotten somebody's happy poop. My whole life is different."
Despite the fact that a fecal transplant is often so successful, current FDA guidelines require that a patient have several occurrences of C. diff before they can receive such a transplant, leaving doctors without many good treatment options.
"To me, it seems a little bit crazy," says Dhere. "Why subject a patient to that much infectious burden if you already know the chance of a reoccurrence is pretty high?"
So Kraft, Dhere, and others are exploring how to extend use of fecal transplants for other patients, using the therapy before C. diff takes its toll.
"We're looking to expand the role of fecal microbiota transplants for other things that are not as severe as C. diff, and maybe closer to a first-line treatment," says Virginia Shaffer, a surgeon on the fecal transplant team.
Shaffer is running an open clinical trial to study the use of fecal transplants to treat pouchitis, an inflammatory condition that affects people who have had a proctocolectomy (removal of part of the colon due to ulcerative colitis).
In a recent article in the American Journal of Infection Control, Kraft and colleagues from Emory and the CDC discuss the need for a microbiome disruption index to inform decisions on antibiotic stewardship and interventions such as fecal microbiota transplants or oral probiotic capsules.
They say that measures of microbiome diversity should assess several factors:
- Overall diversity: how much does one type of bacteria dominate
- Presence of "bad guys," like C. diff
- Presence of "keystone" species that prevent takeover by bad microbes
- Presence of bacteria thought to be beneficial or protective.
Little biome, big data
Microbiome research is one of the fastest growing fields in the biomedical arena largely because the tools to do it—such as DNA-sequencing technologies and computational resources—have gotten so good. "These powerful technologies have come about as a consequence of the human genome project," says Frank Anania, director of Emory's Digestive Diseases Division, who is researching the relationship between a high-fat diet, intestinal microbiota, and non-alcoholic fatty liver disease.
Zwick, scientific director of Emory's genomics and computational core facilities, has a good overview of the diversity of microbiome research being conducted across the university.
"Genomics is the central place where microbiomic sequencing is accomplished. We're generating a massive amount of data for investigators," he says. "We also have a computational core, where the data is analyzed and pipelines are identified. And we're developing a Biostatistics Consulting Center, with a biostatistical cadre for interpretation of this data."
Mouse in a bubble
A recent addition to Emory's microbiome research is the gnotobiotic mouse facility, developed last year by gastroenterologist Rheinallt Jones for his studies into the microbiome's influence on host physiology.
 |
The average mouse, like the average human, is home to trillions of bacteria and viruses. But a mouse in a gnotobiotic facility has no germs on its skin, in its nostrils, or in its gut. Its food, water, and bedding is heated to more than 100°C to kill bacteria and viruses before being delivered to the mouse's cage through a sterile system.
"This facility provides a germ-free environment, so you can study the biology of whole organisms with a complete absence of bacteria," says pathologist Andrew Neish. His research looks at how bacteria contribute to intestinal epithelial integrity and healing.
In the gnotobiotic facility, the microbiome of test animals can be manipulated and defined by researchers.
Jennifer Mulle, a genetic epidemiologist, has studied the microbiome's influence on neural development: in other words, the gut's influence on the brain. "It's the most amazing thing ever," she says. "It really suggests that the microbiome is an essential component of behavior."
The forgotten organ
In her paper, "The Gut Microbiome: A New Frontier in Autism Research," Mulle writes about the Human Microbiome Project, clarifying the initiative's ultimate goal: "To understand how this 'forgotten organ' functions to establish and maintain a healthy state, and whether the microbiome can be manipulated to favor long-term desirable health outcomes."
Interest in the group and microbiome research at Emory spiked after November's two-day microbiome symposium, which brought in experts from Georgia Tech, the CDC, Baylor College of Medicine, University of Michigan, UCLA, Stanford, and Virginia Commonwealth University. The event drew more than 250 people, and Emory plans on making it a semi-annual event, says Mulle, the symposium's organizer.
The Emory Microbiome Group, formed by Kraft, Neish, and microbial genomics expert Tim Read, is thriving, and research studies are taking place across the university. For example, Joanne Goldberg is examining the role of the lung microbiome in cystic fibrosis-related diabetes. "For the longest time, the lung was considered sterile—you didn't think of microbes being there at all," says Goldberg. "But now we appreciate that it actually is a dynamic environment."
Other studies are exploring the role of the microbiome in ALS, bone loss, cancer treatment outcomes, Down syndrome, and epithelial wound repair.
The most ambitious and expansive microbiome research effort so far brought together investigators from the medical, nursing, and public health schools, as well as Emory College and the CDC, for a set of research projects that yielded the creation of the Southeast's first children's environmental health center.
The Center for Children's Health, the Environment, the Microbiome, and Metabolomics (C-CHEM2), formed last fall, is one of 25 children's environmental health centers in the U.S. and the only one focused on the microbiome.
The center grew out of the maternal microbiome project started a few years ago by Emory nursing researchers Elizabeth Corwin and Anne Dunlop. The five-year study seeks to determine how biological and environmental factors influence the microbiome of African American women during pregnancy, and whether disruption of the microbiome causes preterm birth.
African American women have a 1.5 times higher risk of preterm birth than Caucasian women. Nearly 300 women have enrolled so far in the study, which involves the analysis of the participants' microbiota to determine what patterns are linked to preterm births.
 |
An infant microbiome study, co-led by Corwin and Emory psychologist Patricia Brennan, involves a subset of moms from the maternal microbiome project and explores how chronic maternal stress and disadvantage may influence an infant's microbiome. "We want to understand the role of the microbiome in the gut-brain axis," says Corwin, of the biochemical signaling between the digestive tract and the nervous system.
They also want to know more about childhood obesity. "We know that babies born by cesarean section have a different gut microbiome than vaginally born babies, and we know that kids born by cesarean have an increased risk of obesity," says Corwin. "We think that differences in the microbiome may be playing a role."
Diversity rules
These burgeoning studies are just the beginning of exploring the mysterious microscopic worlds within us and the organisms that dwell there.
For years, scientists who studied the microbiome estimated that bacteria outnumbered human cells 10-to-1. Recent calculations put the ratio at something closer to 1.3-to-1.
But this doesn't reduce the huge impact the microbiome has on human health.
"I don't think the number of microbial cells is as important as the diversity of those microbes," Gerardo says. "There are large microbial communities engaging in a tremendous amount of warfare inside of us, competing for and claiming space. Our microbiome helps define who we are, and we're getting to a point where more and more people are realizing that they have an important partnership with their microbes. A healthy, diverse microbiome is a wonderful thing."