Sepsis Survival Skills
By Quinn Eastman, Photography by Jack Kearse

In the summer of 2010, electrical engineer Ketan Thanki was in a specialized intensive care unit at Emory University Hospital, waiting for a heart transplant.
One night, he developed signs of an infection. Because he was sound asleep, he had no idea how dangerous his situation had become.
Thankfully, somebody else did.
"The night nurse woke me up and said I had both a fever of 104 and blood pressure of 60 over 30," he says. "She said she needed to start me on intravenous antibiotics right away."
The nurse had recognized the symptoms of sepsis, an extreme response to infection that can result in organ damage, organ failure, and death. Thanki's low blood pressure was a sign that inflammation within his body was intensifying and affecting his circulation.
The mortality risk for someone who develops sepsis is 15 to 30 percent, higher than the risk for someone who has a heart attack. Sepsis is a leading cause of death in American hospitals and the most expensive condition treated there, accounting for more than $20 billion in health care costs annually.
Due to Thanki's prompt treatment with antibiotics, his infection resolved within a few days and he was able to get the heart transplant he needed.
His experience makes detecting sepsis sound pretty straightforward, yet it sometimes goes unrecognized by medical caregivers until it is too late to intervene effectively.
Sepsis stems from an infection, which then leads to a life-threatening abnormal response of the body to the infection. Pneumonia, urinary tract infections, appendicitis, or an infected scrape could all lead to sepsis.
 |
Symptoms include: shivering, fever or feeling very cold, extreme pain or discomfort, clammy or sweaty skin, confusion or disorientation, shortness of breath, rapid breathing, and high heart rate.
Part of the problem in recognizing sepsis, doctors say, is that it can affect all types of people, and its symptoms don't focus on one part of the body. A sepsis patient can be a young athlete, an elderly person in a nursing home, or a patient in the hospital being treated for something else. "The biggest risk factor is already being sick," says Craig Coopersmith, an Emory critical care specialist who, with colleague Greg Martin, was part of an international effort to redefine sepsis.
The new definition, published in the Journal of the American Medical Association, clarifies terms and clinical criteria to prompt quicker recognition and treatment.
And, perhaps due to rising awareness of the threat, it has proven quite popular: At nearly 1.3 million views, it is currently the fifth most-viewed JAMA paper ever.
 |
Reshaping sepsis care
"If someone's having a heart attack or a stroke, what's happening is easier to grasp," says Coopersmith. "Everyone knows that treatment is urgent in that situation."
Sepsis response, he says, is equally urgent.
In August, the CDC declared sepsis a medical emergency, and reported that about 72 percent of patients with this fast-moving illness had recently been seen by doctors and nurses, representing missed opportunities to catch it.
Consider young Rory Staunton. In 2012, 12-year old Rory cut his arm diving for a basketball at school in New York City. The next day, he went to the emergency department in a hospital there, vomiting and complaining of leg pain. At that time, doctors thought Rory had a simple flu-like illness. He was given fluids, advised to take Tylenol, and sent home. After he left the hospital, results from lab tests showed signs of severe infection in his blood. Three days later, he died of sepsis, despite strenuous efforts to save him.
To avoid such tragedies, academic medical centers like Emory have taken steps toward improving recognition and starting immediate treatment.
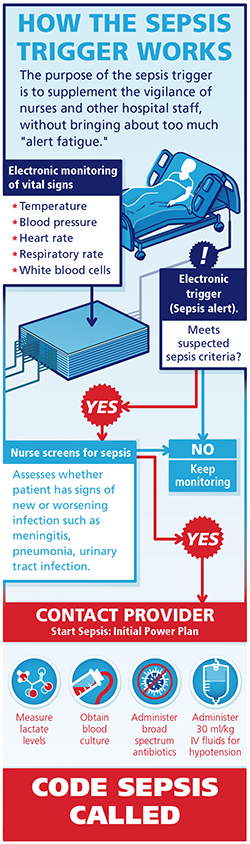
Emory is reshaping how its sepsis care takes place. That means reorganizing teams so that tests and supplies can be delivered more quickly, getting doctors to agree on a standard treatment regimen, and putting into place an "electronic trigger."
The trigger is a computerized version of the perceptive nurse who woke Ketan Thanki up in the middle of the night. Due to Thanki's pending transplant, he was being monitored very closely—his blood was drawn twice a day, and information was being provided to his medical team via a Swan Ganz catheter in his heart. So when Thanki developed signs of infection, hospital staff detected it right away.
The purpose of the electronic trigger for sepsis is to broaden that monitoring so that patients all over the hospital, not just in an intensive care unit, can be caught in its safety net.
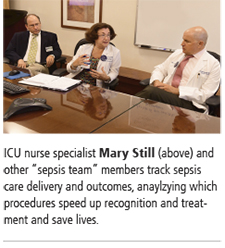 |
"Before, patients in the ICU were screened every 12 hours, but many opportunities were missed," says Mary Still, a clinical nurse specialist in the surgical transplant ICU. Still, along with colleague Carolyn Holder, a clinical nurse specialist in the medical ICU, has led the charge on early recognition and treatment of sepsis.
The trigger checks patients' vital signs. If they indicate a potential problem, it sends an alert to the nurse on duty to evaluate the patient for signs of infection or impaired organ function.
This is nuts and bolts stuff and doesn't involve introducing new medicines or procedures that doctors or nurses are unfamiliar with. After many clinical studies, the only measures proven to help patients fight sepsis are antibiotics and fluid replenishment.
"The things that we need to do haven't changed," says critical care quality expert David Murphy. "We want to reduce the number of clicks and steps needed to do the right thing."
As mundane as the phrases "electronic medical record" or "computerized provider order entry" may sound, this is an area where harnessing their power is expected to make a significant difference.
"Getting the orders computerized, that was huge. It was all on paper before," Still says. "I didn't realize the impact of culture and silos of information until I got involved in this process."
Emory has customized its approach to minimize "alert fatigue," Murphy says, which is when medical teams are asked to pay attention to so many alarms, alerts, beeps, and buzzes they get overwhelmed.
The Centers for Medicare and Medicaid Services requires that hospitals collect data on "bundles" that specify what medical teams are supposed to do for patients with sepsis within three and six hours after time of presentation.
"A challenge was persuading doctors to view the sepsis bundles as 'set menus' rather than 'a la carte,' " Still says.
The three-hour bundle calls for a relatively simple set of actions, which Coopersmith and other sepsis experts have been promoting:
1 Measure lactate, an indicator of sepsis.
2 Test for bacteria in the blood.
3 Administer broad-spectrum antibiotics.
4 Give fluids if blood pressure is low or lactate is high.
After the trigger was implemented last year, sepsis protocol adherence increased substantially at Emory's four hospitals, to 77 percent.
Benefits have included a reduction in patient length of stay and more discharges home instead of to a rehab or skilled nursing facility.
"I think these measures are going to save thousands of lives, nationwide," Coopersmith says.
Achieving flow
Emory Healthcare team members with an interest in sepsis care have been meeting regularly to discuss tactics and results.
When they started getting everybody together, they realized there were six different protocols for sepsis treatment on Clifton Road alone, between the emergency department, the ICUs, and the wards.
"It took a year to get everyone on the same page," says Jonathan Sevransky, who oversees the medical intensive care unit at Emory University Hospital. "Even if we have computers, we can't forget about personal communication."
 |
For process re-engineering of this kind, physicians, nurses, pharmacists, technicians, and others must work together. "We have to persuade people that these are important guidelines to follow and give them data on their performance. We haven't shoved anything down people's throats—it's more, 'Can you live with this?' "
Sepsis survivors are an important part of the prevention and recognition efforts. After Ketan Thanki's recovery from sepsis, and heart transplant, he became a patient-family adviser at Emory Healthcare.
Volunteer advisers are current or former Emory patients or family members who help improve care by weighing in on everything from policy development to hospital design. Several have taken a special interest in sepsis care, preparing educational materials on infection prevention and on how to recognize sepsis at home.
It's all about increasing awareness, says Sevransky. "I tell our trainees, if I'm the one to diagnose sepsis, we failed. My job is to make sure other people do it instead of me."
Full-Court PRESS
A landmark study of more than 2,000 sepsis patients showed that for every hour of delay in providing antibiotics, the mortality risk went up by about 8 percent.
One way to cut delays would be to recognize that a patient coming to the hospital has sepsis—before they even get there.
 |
Critical care specialist Carmen Polito notes that diagnosis of a severe heart attack is now often made by paramedics, allowing the cardiac catheterization lab to be activated before the patient reaches the hospital. She'd like to see something similar be achieved for sepsis, allowing immediate triage.
Polito and a multidisciplinary team including Arthur Yancey, medical director of Grady Emergency Medical Services, are developing tools to help EMS providers do exactly that. They analyzed Grady EMS data from 2011 and 2012, looking for information available to first responders that could have predicted which patients had sepsis. Unaided, the responders detected sepsis about 20 percent of the time.
"Sepsis is largely a face without a name in the EMS setting," Polito says. "The goal of our study was to create a tool to assist EMS providers in naming this deadly condition at the point of first medical contact." Her team built a model that works like this: some patients are defined as "at risk" based on their heart rate, breathing rate, and blood pressure. For those patients, a risk score (PRESS, for prehospital recognition of severe sepsis) is calculated, using several criteria that can be measured quickly and noninvasively.
Polito's team used a complicated algorithm to determine someone's PRESS score. During the fall, Grady EMS will be testing this sepsis screening in the field. Yancey, Polito, and colleagues will train more than 300 first responders on how to use PRESS. For on-the-street implementation, the algorithm has been simplified so that the presence of all three of the indicators, along with any of six risk factors [older than 40, transport from nursing home, EMS flag for sick person, elevated temperature by touch, very low systolic blood pressure, or low oxygen saturation] will trigger a sepsis alert. At that point, EMS providers will start giving the patient intravenous fluids and notify the receiving hospital by two-way radio.
"This tells the emergency department that, even if they are having a busy night, this person's care should be prioritized," Yancey says.
Lost in Translation?
Because of vaccinations and infections, your immune system accumulates memory T cells, which enable it to respond effectively to bacteria or viruses it has seen before.
Not so with mice kept in clean laboratory facilities. Emory scientists think this difference could help explain why treatments for sepsis that work in mice haven't had the same success in human clinical trials. "This is an issue we've been aware of in transplant immunology for a long time," says Mandy Ford, scientific director of Emory Transplant Center. "Real-life humans have more memory T cells than the mice that we study."
Ford has teamed up with Craig Coopersmith to investigate sepsis, a relatively new field for her, and the collaboration has blossomed.
Sepsis is like a storm moving through the immune system. Scientists studying sepsis think that it has a hyper-inflammatory phase, and a phase of impaired immune function afterward. The ensuing paralysis leaves patients unable to fight off secondary infections. In late-stage sepsis patients, viruses that the immune system usually keeps under control, such as Epstein-Barr and cytomegalovirus, emerge from hiding. The situation resembles that of kidney transplant patients, who are taking drugs to prevent rejection of their new organ, Ford says. It was recently discovered that sepsis preferentially depletes some types of memory T cells in mice. Because T cells usually keep latent viruses in check, this may explain why the viruses are reactivated after sepsis, she says.
Ford and her team have been focusing on a molecule called 2B4, which is found on memory T cells, regulates their function, and is more abundant during sepsis.
In a mouse model of septic infection, 85 percent of normal mice usually die, but 13 percent of mice lacking 2B4 died. This suggests that a treatment that could block 2B4 from functioning could provide a survival benefit. Ford's team is poised to try 2B4 experiments with "memory mice," which have cleared several infections and thus have immune systems that resemble those of adult humans more closely.
The observations of impaired immune function in late-stage sepsis have led to proposals to try immunotherapy drugs, which wake up exhausted T cells to fight cancer. A clinical trial of one such agent is under way at Emory. "It's the opposite of what everybody has been trying for the past 30 years, but it does make sense in light of these recent findings," Ford says.
 |
In addition, Ford and Coopersmith have been investigating the possibility that not every sepsis patient should be treated the same. The presence of cancer, for example, may so distort the immune system that anti-sepsis treatments that have proven beneficial in previously healthy mice become harmful. Chronic alcohol ingestion may have similar distorting effects.
"We're adding in comorbidities that reflect the human condition," Coopersmith says.