The Anatomy of Fear
By Martha McKenzie, Illustration by Brian Stauffer
 Fear in a mouse brain looks much the same as fear in a human brain.
Fear in a mouse brain looks much the same as fear in a human brain.
When a frightening stimulus is encountered, the thalamus shoots a message to the amygdala—the primitive part of the brain—even before it informs the parts responsible for higher cognition. The amygdala then goes into its hard-wired fight-or-flight response, triggering a host of predictable symptoms, including racing heart, heavy breathing, startle response, and sweating.
The similarities of fear response in the brains of mice and men have allowed scientists to understand the neural circuitry and molecular processes of fear and fear behaviors perhaps better than any other response. That understanding has spurred breakthroughs in treatments for psychiatric disorders that are underpinned by fear.
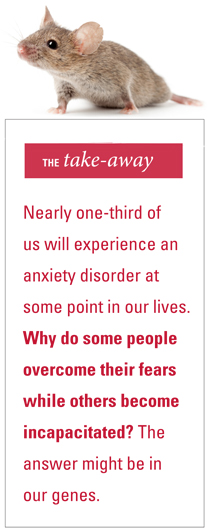
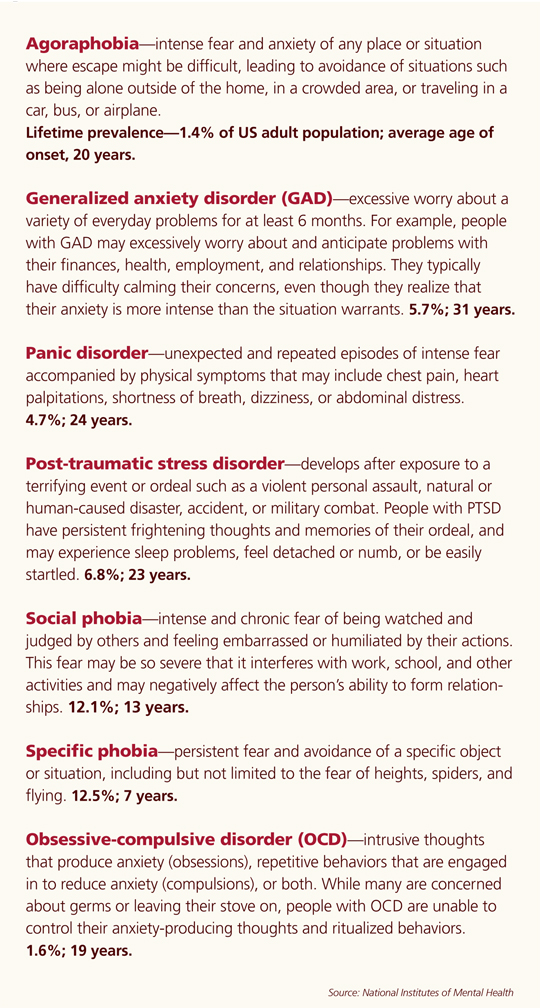
Anxiety disorders are one of the most common mental illnesses in the country, with nearly one-third of Americans experiencing symptoms at least once during their lives. There are generalized anxiety disorders and fear-related disorders, which include panic disorders, phobias, and post-traumatic stress disorder (PTSD).
Psychiatrist and researcher Kerry Ressler is on the front lines of fear-disorder research. In his lab at Yerkes National Primate Research Center, he studies the molecular and cellular mechanisms of fear learning and extinction in mouse models. At Grady Hospital, he investigates the psychology, genetics, and biology of PTSD. And through the Grady Trauma Project, he works to draw attention to the problem of inner city intergenerational violence.
 |
|
|
Psychiatrist Kerry Ressler studies the molecular and cellular mechanisms of fear learning and extinction to determine the role biology plays in placing people at risk for anxiety disorders, phobias, and post-traumatic stress disorder (PTSD); he's also researching the genetic transfer of fears and phobias across generations. Courtesy of Kerry Ressler
|
|
"If you look at Kerry's work, it can seem like it's all over the place—he's got so many studies going on, and he collaborates with so many other scientists," says Barbara Rothbaum, associate vice chair of clinical research in psychiatry and director of the Trauma and Anxiety Recovery Program at Emory. "But they are all pieces to the same puzzle. All his work, from molecular to clinical to policy, fits together and starts telling a story." A Howard Hughes Medical Institute investigator, Ressler was recently elected to the Institute of Medicine—one of the highest honors in the fields of health and medicine. He was named a member of a new national PTSD consortium led by Draper Laboratory. And he recently appeared on the Charlie Rose show's brain series.
"There's a patient I've seen who was attacked in a dark alley," Ressler shared on the show. "Initially it just felt dangerous to go out at night, but after a while she grew afraid of men and couldn't go to that part of town. Then she couldn't leave her house, and finally, her bedroom. The world got more and more dangerous."
Amygdala-based anxiety
Ressler wanted to see if he could identify genes that could explain why some people (about 20%) develop PTSD after a trauma while others are resilient.
He traumatized a group of mice—immobilizing them by strapping them to wooden boards for two hours. A week later, he put both the traumatized group of mice and a control group that had not undergone trauma through a common fear-conditioning regimen. Mice received a slight shock on their feet at the same time that a tone sounded. Days later he played the tone without an accompanying shock, and some of the previously traumatized mice exhibited PTSD-like symptoms. They startled more dramatically and were unable to "extinguish" their fear—to learn that the tone was now safe and no longer signaled a shock.
When the region of the brain responsible for creating and storing fear memories, the amygdala, was examined afterward through autopsies, Ressler and researcher Raul Andero found that one gene, Oprl1 (opioid receptor-like 1), was switched on in the mice that had experienced prior trauma and had PTSD-like symptoms. "From that finding, we hypothesized that if we could activate the Oprl1 pathway within the brain, it would prevent the over-learning of the fear response, which is at the crux of the PTSD syndrome," says Ressler.
A literature search revealed only two papers looking at this gene and its pathway in humans, and Ressler happened to know the author of one from Scripps Research Institute. He contacted Scripps and found that its institute, along with University of Miami, had developed a drug called SR-8993 that targets the Oprl1 receptor. The pathway is part of a family of opioid receptors that allow brain cells to receive signals from opioid drugs as well as natural opioids produced by the body. Scientists, however, believe that the euphoric and analgesic effects of opioid drugs mainly come from triggering other members of the opioid receptor family, not Oprl1. As a result, Scripps was looking at the drug as a possible treatment for drug and alcohol addiction.
Ressler's team repeated all the steps from the first mouse study, but this time they administered SR-8993 after fear conditioning. The previously traumatized mice that got the drug did not develop any of the PTSD symptoms. They behaved like their control kindred.
"We think SR-8993 is helping promote a natural process that occurs after trauma, preventing fear learning from becoming over-represented and generalized," Ressler says. "Our model is that in PTSD, the Oprl1 system is serving as a brake on fear learning, but that brake is not working if prior trauma had occurred. This is an important step toward developing a treatment to possibly prevent the onset of PTSD symptoms."
Previous studies in Ressler's lab, in collaboration with Michael Davis, emeritus professor of psychiatry, showed it was possible to prevent the development of PTSD-like fear memories in rats by doing extinction training immediately after a trauma, since a memory doesn't become permanent, or consolidated, right away. So directly after going through the shock/tone fear conditioning, the rat is repeatedly exposed to the tone without the shock and doesn't learn to fear the tone.
In collaboration with Rothbaum and Debra Houry, vice chair for research in emergency medicine and director of the Emory Center for Injury Control, Ressler set out to see if the same window of time existed in humans. Patients admitted to the ER following a trauma—a car wreck, gunshot wound, rape—received imaginal exposure therapy. "We asked them to talk about what happened to them in a therapeutic way," says Rothbaum. "We know this type of cognitive behavior therapy works very well for people with chronic PTSD. Here we were applying the same technique before the fear memory was consolidated."
The results were encouraging. Three months after their trauma, PTSD incidence in patients who received the intervention was half that of patients who did not receive it.
"This is significant because some earlier studies had shown that psychological de-briefing could actually make people worse, which scared people off from early interventions," Rothbaum says. "The fact that our intervention worked so well may help reopen early intervention efforts."
Predicting and Preventing PTSD
Ressler and his team are taking this study a step further, collecting blood samples from trauma victims in the ER and searching for genes and other biomarkers that would identify people who are at increased risk for developing PTSD following trauma.
 |
|
|
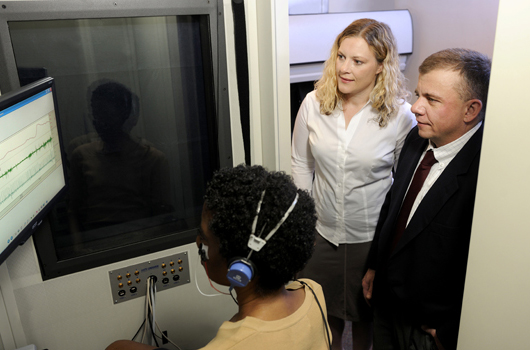
Shown here at the "startle booth" at the Atlanta VA Medical Center, Tanja Jovanovic, assistant professor of psychiatry, and Bekh Bradley, cofounder of the Grady Trauma Project and director of the PTSD treatment program at the VA, are collaborating with Ressler on a research study involving highly traumatized mothers with and without PTSD, and their children. "We are looking at psychological, physiological, and genetic components of both the mothers and their children and then following them over time," Jovanovic says. Photo by Jack Kearse
|
|
So far pilot data from the study agree with findings reported in two recent papers—people who get morphine immediately after a trauma are less likely to develop PTSD. Many assume that's because morphine is an analgesic, so the patients who get it do not experience the pain as severely and therefore are less likely to develop PTSD. But Ressler hypothesizes that morphine's protective powers stem from activating the Oprl1 gene pathway in the amygdala.
"In the same way we found these brain-based biomarkers in mice that changed right after a trauma or fear conditioning, we are getting blood from people right after they come into the ED and looking for biomarkers that are predictive, within the first hours after suffering a trauma, of later development of PTSD," says Ressler. "The vision would be to develop the equivalent of a stroke protocol or a heart attack protocol in the ED for psychological trauma."
Based both on answers to a set of psychological questions and on blood-based biomarkers, he says, predictions could be made about who is at highest risk of developing PTSD. With early pharmacological or psychological therapeutic intervention, possibly even in the emergency department, preventing PTSD might be possible.
People tend to equate PTSD with combat trauma, and, in fact, most PTSD research, treatment, and funding is focused on returning veterans. Yet Ressler and his colleagues have found that low-income, inner-city residents suffer from the disorder as much as or more than combat vets.
"One of the reasons we created the Grady Trauma Project and continue to work on it is to shine light on an extremely underserved and underappreciated problem, civilian inner-city trauma," says Ressler. "Within the Grady Hospital population, we've found that 80% to 90% have experienced a severe trauma, and 30% to 35% have gone on to develop PTSD. That rate is higher than for combat vets, yet this is something that most people are not aware of. We think it is an epidemic problem, and we believe that the inner-city cycle of violence and poverty can be explained in part through the effects of trauma on residents' brains."
The Grady Trauma Project is now in its seventh year, and DNA, historical, and psychological data have been collected on more than 6,000 Grady medical clinic outpatients. "These are not patients from the ED or from psychiatry," says Ressler. "We wanted a cross-sample of the general Grady patient population."
Ressler and his team are examining subjects' genomes to look for PTSD risk factors. "We currently understand what a few hundred of the genes in the brain do," he says. "But that's only about 2% of the brain's expressed genes. We don't know how the vast majority of these work. Looking at the entire genome likely will allow us to identify other important genes involved."
The Grady project may also shed some light on the intergenerational nature of PTSD. In collaboration with Tanja Jovanovic, assistant professor of psychiatry, and Bekh Bradley, co-founder of the Grady Trauma Project and director of the PTSD treatment program at the Atlanta Veterans' Affairs Medical Center, Ressler is looking at highly traumatized mothers with and without PTSD and their children. "We
are looking at psychological, physiological, and genetic components of both the mothers and their children and then following them over time," Jovanovic says.
Scientists know that about 30% to 40% of the risk for PTSD is inherited. They speculate that genes shared between parent and child may be one mechanism for this inheritance, or that traumatized parents could increase their children's likelihood of developing symptoms environmentally, through psychological and parenting processes.
Another interesting answer could lie in the new science of epigenetics. "A mother's stress could alter gene expression from her own DNA through experience-dependent chemical 'tags' on her DNA, which she could then also pass down to her child," says Ressler. "So we think evidence is building that experiences in one generation could affect how genes are expressed in the next generation."
Fears of our fathers
Ressler's lab at Yerkes is following up on some of these ideas in powerful mouse models of epigenetic transfer of fear across generations.
Ressler and fellow researcher Brian Dias trained mice to become afraid of an odor by pairing exposure to the odor with a mild electric shock. They then measured how much the animal startled in response to a loud noise alone, and then in conjunction with the odor.
Surprisingly, they found that the naïve adult offspring of the sensitized mice also startled more in response to the particular odor that one parent had learned to fear, despite the fact that they had never been exposed to the odor/shock combination.
In addition, the younger mice were more able to detect small amounts of that particular odor.
A third generation of mice also inherited this reaction, as did mice conceived through in vitro fertilization with sperm from males sensitized to the smell.
These offspring were not more anxious in general; in separate experiments not involving odors, Dias found that the mice were not more afraid to explore the bright, elevated areas of a maze.
Dias also discovered that the DNA from the sperm of the smell-sensitized father mice is altered. This is an epigenetic alteration, found not in the letter-by-letter sequence of the DNA but in its packaging or chemical modifications.
Knowing how the experiences of parents influence their descendants helps us understand psychiatric disorders that may have a transgenerational basis and possibly to design therapeutic strategies, Ressler says.
"Practicing medicine reminds us of why the research we do is so important for our patients, who are suffering every day," he says. "And if we find ways to treat these adults, it may very well help their children and grandchildren as well."
![]()
To see Kerry Ressler speak about the neuroscience of emotion at TEDx Peachtree 2012, go to tedxpeachtree.com/tag/kerry-ressler. To see Ressler on the Charlie Rose show's brain series, go to charlierose.com/watch/50059537.