Can Choice Change Pain?

The pain education I received in the '90s came from Oxycontin-sponsored lunches. Over lasagna and green salad, I learned I could use opioids to get patients pain-free after surgery or trauma, with no risk of addiction. I wore a "NO PAIN" pin and researched and lectured on analgesic options. American medical schools average only 12 hours of pain curriculum, almost exclusively pharmacology, so to me "options" meant pharmaceuticals. And while the addiction part has been debunked, many trained in my era still believe in a pain-free goal and a pill as the path.
After 20 years of practice, three decades of opioid disillusionment, and $4 million in National Institutes of Health (NIH) funding, I now believe that nonpharmacologic options work better than opioids. Rather than a quantitative 0–10 scale, new fMRI findings support addressing pain as a complex interplay of physiology and experience, where fear and control are the volume knobs for a qualitative personal experience.
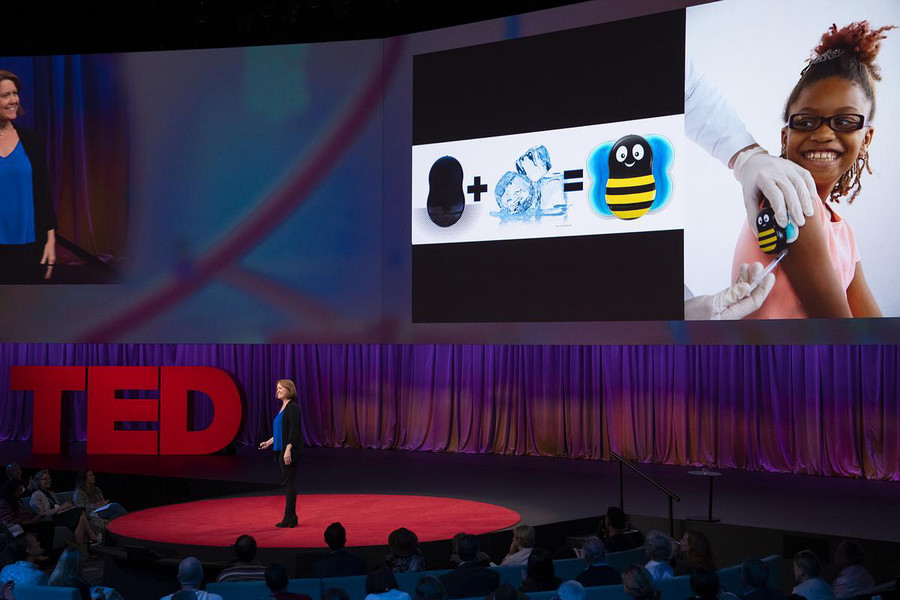
My pain research journey began with topical anesthetics for lumbar punctures, or more specifically, an attempt to increase their use in neonatal septic workups. In pediatric emergency medicine, we rarely had time for topicals to work for IVs, and the data for injections is still scant. I wanted a faster solution, emulating how running water soothes a burn or rubbing a bumped elbow stops pain. The mechanism by which motion inhibits nociceptor (sensory receptors for pain) firing is called "spinal gating." In 2009, I received my first NIH grant to investigate this using a cold, vibration device for vaccination pain. Full disclosure, I now invent and research thermomechanical neuromodulation devices.
During this time my pro-opioid lecturing about emergency analgesics grew increasingly dissonant from my clinical observations. While topical anesthetics and my device, "Buzzy," worked equally well for IV access, both were equally useless for older children in the face of fear: even the alcohol swab elicited screams. For terrified adolescents with tattoos or piercings, the issue clearly wasn't the needle.
We also found that for sickle cell patients with intense pain crises, talking on the phone to a friend could take the edge off while we put in a line for morphine.
The answer to this pain paradox came from a director of Child Life at a hospital in Wisconsin. Child life specialists explain medical equipment and tests to young patients and use precise types of distraction to reduce procedural pain.
The director had invited me to deliver a grand round, so her team would know how to advocate for their patients. She also understood pain on a deeply personal level, after a lifetime of rheumatoid arthritis, hundreds of surgeries, and a decade of using crutches or a wheelchair, depending on the day. On this overcast day, as we left the conference center, she needed her wheelchair. I asked which medications helped her most.
"Honestly, not many," she said. "I look at it like an inverted pyramid: there are very few pharmaceuticals that can stop the disease that causes my pain. There are over-the-counter pills or supplements or food choices that can make the pain more manageable. Those aren't usually enough, but there are even more physical options I can try — exercise, movement, heat, massage. And most of all, there are an infinite number of combinations of ways to make my brain ignore pain: friends, activities, faith, entertainment, music. Feeling helpless or afraid makes pain worse, so the most important way I deal with pain is always having another option."
Despite my growing awareness of nonphysiologic impacts on pain, I was still espousing opioids for outpatients and still believed they were "not addictive if you're really in pain." I was surprised they weren't a mainstay for the child-life director. Over the next few years, research echoed her experience: home opioids were less effective than ibuprofen for fractures, wisdom teeth removal, and other outpatient procedures.
When a colleague in recovery used my device to avoid home opioids after a total knee replacement, my path changed. I'd lost a friend in high school to a heroin overdose, yet still perceived addiction to be a moral failing rather than a genetic predisposition. Learning that a brilliant friend had opioid-use disorder made me reconsider. Moreover, if the option of vibration and cold could prevent the descent into loss and darkness for even a few people, it was worth the risk of leaving clinical practice to understand how. In 2016, I moved to full-time research to translate this science into an opioid-sparing clinical device, starting from scratch — whatever central pain physiology I'd learned was long gone.
The original stimulus for Melzack and Wall's 1965 Gate Control Theory was precisely calibrated mechanical stimulation — vibration. Spinal gating happens when Pacinian nerve endings (sensory receptors for vibration and proprioception) send three-dimensional tactile information to the dorsal horn. Pacinians, it turns out, are 90% of the mechanoreceptors that release neurotransmitters directly in the spine, and the only ones that inhibit acute pain. Vibration isn't just a distraction — the dorsal horn pain neurons stop firing.
In the early 2000s, the pathways by which cold caused descending inhibition from the thalamus to reduce pain perception were described. But the clincher came from fMRI discoveries in the past decade. Even with no pain stimulus at all, resting "connectome" patterns in the brain predict pain intensity. The anticipation of a needle jab connects brain regions for sensations, memories, fear, agency, choice, expectation, and focus, causing pain even when a fake arm is poked. Some of what we feel is what we're conditioned to feel, amplified by fear. Pain is dynamic. Pain is subjective. Rather than an absolute sensation, pain is your brain's best guess of safety. If patients understand what to expect, fear is reduced, and pain is more manageable. Activities that require certain kinds of concentration prioritize the brain's connection hub, so fear, experience, or expectation aren't activated and pain is reduced.
Practicing with a physical intervention to know how much relief to expect increases the feeling of control and decreases fear. Brain-body distractions, and reducing fear with a pain plan, lets patients tolerate more pain for longer. Having options addresses fear, physiology, and control.
Amy Baxter’s TED talk, “How to hack your brain when you’re in pain,” has received more than 1.1 million views.
For inpatients in the wake of surgeries, trauma, and pain disorders, opioids reduce PTSD and chronic pain. Opioids activate reward centers all over the brain's pain connections, but with acute use the mu-receptor activation declines in days. Adequately treating acute in-house pain and already established chronic opioid use aren't fueling our national crisis — unneeded or prolonged oral opioids prescribed after surgery are.
Opioid prescribing is dropping, but the US health system doesn't yet pay for supplements, physical options, coaching, or cognitive distractions to replace them. With the mechanical stimulation neuromodulation science, data showing opioid reduction, and a better understanding of the brain, there's hope.
For now, if we help surgical patients aim for "more comfortable" rather than "pain-free," encourage options rather than opioids, and gather a few physiology-fear-control tricks, we can teach patients how choice changes pain.
Amy Baxter is an alumna of Emory School of Medicine and chief medical officer and CEO of Pain Care Labs.