Every Mother, Every Baby

Biomedical engineer Gari Clifford and anthropologist Rachel Hall-Clifford, were their own first test subjects for a device they invented that helps assess maternal and fetal health.
Living in the United Kingdom at the time, they had been keeping tabs on their first child in utero with a borrowed fetal monitor. They realized such low-cost monitoring of pregnant women could be helpful, especially in countries where prenatal care is minimal.
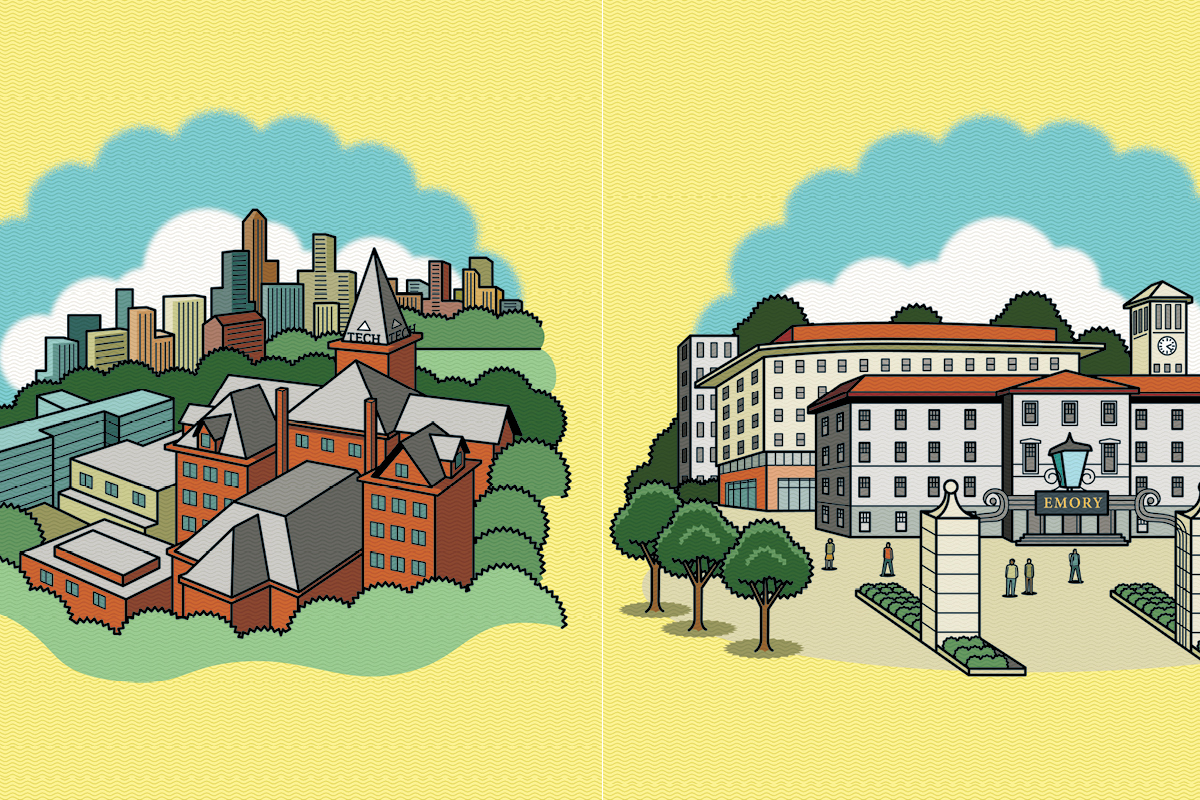
Clifford, chair of the biomedical informatics department at Emory, immediately saw the potential of smartphones and wearable fitness devices to gather personal health data and use it to signal individual health warnings or to track public health trends.
And the prevalence of smartphones solved one of the challenges of health care technology—that it’s prohibitively expensive.
Clifford looks for easier, cheaper ways to get results. For example, while doing fieldwork in South Africa, he used a 25-cent egg cup with a hole drilled in it to replace a stethoscope.
He applied the same logic to a prenatal monitoring kit. The kit, called safe+natal, uses a smartphone, a small doppler ultrasound device, blood pressure cuff, pulse oximeter, and speaker. Two headphone jacks, one for the cell phone and the other for a speaker, amplify the heartbeat. Each kit costs about $200.
Field Test Hall-Clifford lived in Guatemala while doing field research on childhood diarrheal diseases: “I became aware of all the challenges to health care delivery. Gari would visit, and Guatemala pulled us in. We fell in love with the place and the people.”
Women in Guatemala have one of the highest rates of maternal mortality in Latin America. In rural communities, up to 75 percent give birth at home with midwives and often have difficulty getting care in medical facilities. “We provide good critiques of each other’s work. Rachel holds my tech accountable.” Gari Clifford
They developed their kit with a local non-governmental organization, the Maya Health Alliance. By this point, they had an enormous database of some 20,000 recordings.
“Our son is part of the archive,” Clifford says. Being able to set normal baselines allowed them to pick up on warning signals. The smartphone application records and securely transmits patient information for review by clinical staff, flagging serious complications for immediate follow-up. The safe+natal program, developed with funding from NIH and the Charles Hood Foundation, includes regular monitoring and 24-hour access to clinical support from Maya Health Alliance. The device is now used by about 42 midwives in rural Guatemala.
“We aren’t just cooking something up here and dropping it off there,” says Hall-Clifford. “We developed a shared vision and goals with the midwives and the patients.”
CO-Design Clifford and Hall-Clifford share a lab and teach classes at Emory on co-design for resource-constrained settings. As a visual aid, Clifford will often pull out a can opener used in the Vietnam War…one piece, with a hinge, easy to manufacture. “You can keep a can opener with you at all times, and you’ll have a weight and a viable tool. It’s a piece of tech just as much as fancy electronics.”
Hall-Clifford adds, “The control arm for our safe+natal kit was actually a piece of paper with all the steps on it. A crazy little part of me was rooting for the paper. Tech for tech’s sake doesn’t serve any purpose.”
The safe+natal app is made to be as simple and user-friendly as possible. Local midwives modeled for the photos. “A help button tells you what you should do next. It requires zero literacy. We pretend the manual exploded,” Clifford says. The best part, they say, was their last international trip before COVID, when they met with midwives in Guatemala who presented the program back to them, talking the couple through the safe+natal kit. “It was all theirs,” Hall-Clifford says. The kit has become the standard of care there and several years later is still growing. They have plans to expand the program—in the near term, to the southeastern US. “Here in Georgia, we have the highest maternal mortality rate in the US,” Hall-Clifford says. “The same principles are applicable here at home.” The are beginning the Co-Design Lab for Health Equity in Emory’s Center for the Study of Human Health. “We want to expand safe+natal and use co-design to broaden our reach."